1. Patient Introduction
-
Chief Complaint (CC)
-
Age, gender, and brief context (e.g., “Mr. Smith, a 52-year-old male, presents with chest pain.”)
2. History Taking
a. History of Present Illness (HPI)
-
Onset, Location, Duration, Character, Aggravating/Alleviating factors, Radiation, Timing, Severity (OLDCARTS)
-
Associated symptoms
b. Past Medical History (PMH)
-
Chronic conditions, surgeries, hospitalizations
c. Family History (FH)
-
Genetically linked conditions (heart disease, diabetes, cancer)
d. Social History (SH)
-
Smoking, alcohol, drug use, occupation, living conditions
e. Medications & Allergies
-
Current medications, herbal supplements
-
Known drug/food/environmental allergies
3. Review of Systems (ROS)
-
Head-to-toe symptom checklist by system (e.g., cardiovascular, respiratory, GI, neuro)
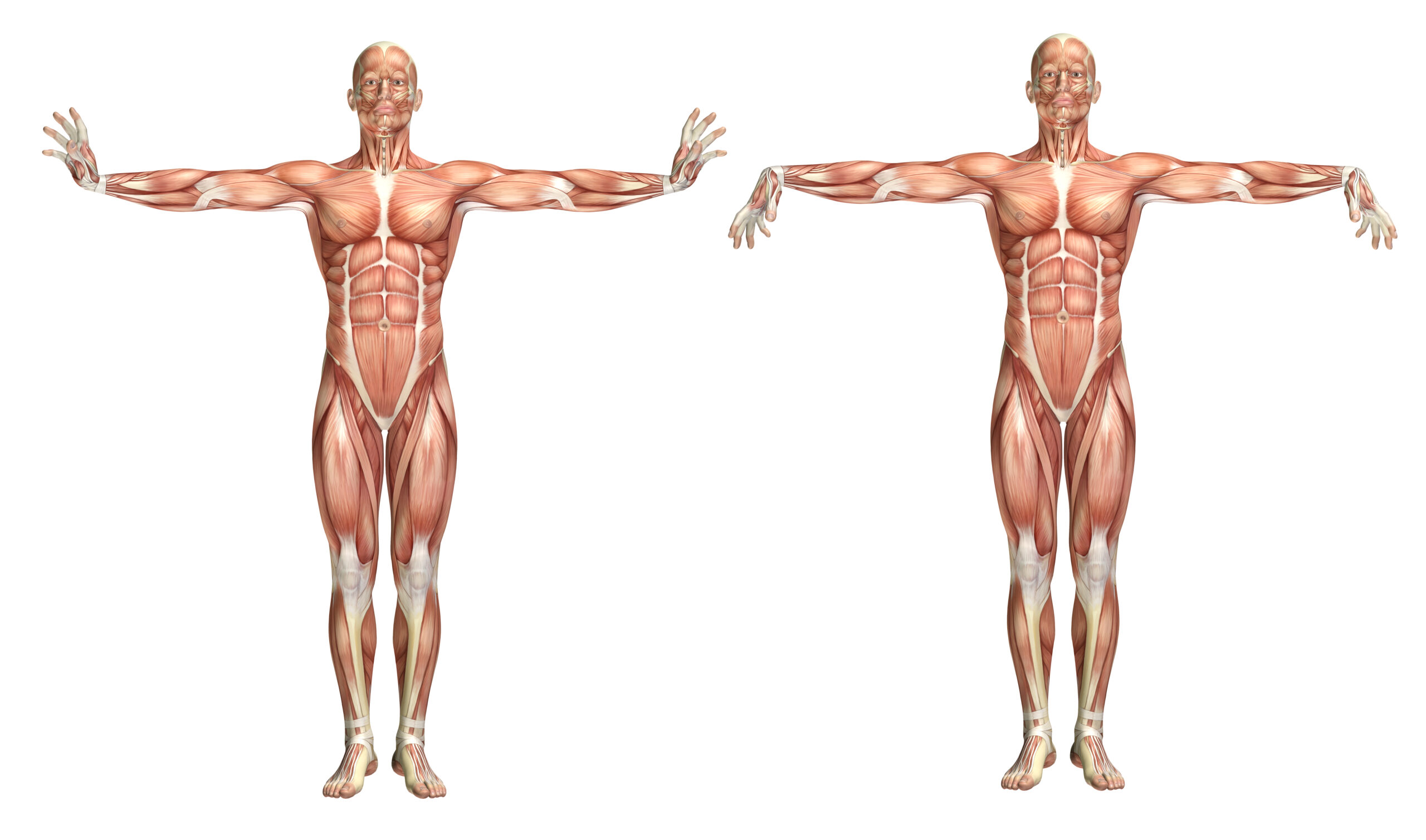
4. Physical Examination
-
Vital signs (BP, HR, RR, Temp, O2 Sat)
-
Focused systems exam
-
General appearance
-
Heart & lungs
-
Abdominal
-
Neuro/MSK as needed
-
-
Identify abnormal findings
5. Differential Diagnosis (DDx)
-
List 3–5 possible diagnoses
-
Rank by likelihood
-
Justify each with signs/symptoms
6. Diagnostic Workup
-
Labs (e.g., CBC, CMP, troponin)
-
Imaging (X-ray, CT, MRI, US)
-
Other tests (ECG, PFTs, cultures)
7. Final Diagnosis
-
Confirmed by test results and clinical evidence
8. Management Plan
a. Pharmacologic
-
Drug name, dose, route, frequency, duration
b. Non-Pharmacologic
-
Lifestyle changes, physical therapy, counseling
c. Patient Education
-
Diagnosis explanation, medication use, red flags
d. Follow-up
-
Timeline and goals for reassessment
9. SOAP Note Documentation
-
Subjective: HPI, ROS, PMH, SH, FH
-
Objective: Vitals, physical exam, labs/imaging
-
Assessment: DDx → final diagnosis
-
Plan: Diagnostics, treatment, education, follow-up
10. Reflection & Clinical Reasoning Feedback
-
What went well?
-
What did you miss?
-
What would you do differently?